The Unfinished Promise: Every Mother, Every Newborn, Thriving
Maternal mortality is more than a statistic; it’s a human rights crisis, a heartbreaking symbol of health inequity, and a tragedy that is almost entirely preventable.
Across Asia and the Pacific, the journey into motherhood is too often overshadowed by the devastating risks of death or injury during childbirth. Despite global commitments, progress in saving mothers’ lives has slowed since 2016, leaving millions vulnerable.
At UNFPA, we believe every woman deserves to not only survive childbirth but to thrive. Our global strategy, Start with Her (2025–2030), is our unwavering commitment to this belief. We are urgently working towards the global goal of reducing maternal deaths to fewer than 70 per 100,000 live births by 2030. The time to act is now.
Our maternal health strategy is built upon four core pillars, designed to accelerate progress towards ending preventable maternal deaths and ensuring that every woman experiences a safe and healthy journey to motherhood.
- Commit to Action: UNFPA works to secure vital funding, strengthen legal frameworks, and drive policy changes to close the global investment gap and embed maternal health as key national priority across Asia-Pacific.
- Deliver Quality Care: UNFPA strives to provide accessible, high-quality health services by expanding emergency obstetric and newborn care (EmONC) and building a stronger, more skilled health workforce - focused on midwives.
- Empower Women: UNFPA’s focus is on ensuring women’s rights and wellbeing by promoting respectful care, addressing mental health needs, and supporting women’s ability to make informed choices on their sexual and reproductive health.
- Leverage Data: UNFPA strengthens accountability through maternal mortality surveillance systems (MPDSR) to gather crucial data, driving continuous quality improvement and promoting equity in maternal health.
Priority 1: Commit to Policy and Investments
This priority addresses the need for robust financial and legal frameworks to accelerate the reduction of maternal mortality and morbidity. Making motherhood safer is a human rights imperative and is central to UNFPA’s mandate. Globally, a critical $104 billion funding gap remains to end preventable maternal deaths by 2030.
The best policy solution is investing in high-quality maternal care, centred around midwives. Fully trained midwives are positioned to provide 90% of all essential sexual, reproductive, maternal, and newborn health services. Policy support for midwifery models of care yield strong economic and social benefits, delivering an estimated $16 return for every $1 invested.
Policy Imperatives for Maternal Health
UNFPA works to deepen the integration of maternal health in national laws, policies, and programmes, guided by universal human rights standards. This includes strengthening the health system environment through policy action in three key areas:
- Strengthening the Midwifery Workforce: UNFPA prioritizes policies that ensure the maternal health workforce is well-trained and qualified, supported, and positioned to deliver high-quality care, aligning with the Global Midwifery Accelerator by:
- Ensuring high-quality education aligned with midwifery global standards
- Advancing professional education to maintain skills, especially in emergency obstetric and newborn care
- Upholding Rights, Wellbeing, and Resilience: UNFPA focuses on ensuring delivery of compassionate, rights-based care, and proactively addresses challenges in achieving high-quality care.
- Advocating for policies that enforce human rights standards, ensuring access to safe, quality, respectful and affordable care
- Policies that support efforts to eliminate significant reproductive morbidities, such as Obstetric Fistulas and cervical cancer, and promote the integration of maternal health into planning for climate resilience.
- Ensuring Financial investments and Accountability: UNFPA leads the development and generation of evidence-based advocacy to ensure maternal health is financed and monitored effectively.
- UNFPA advocates for the full integration of SRHR and maternal health services into Universal Health Coverage (UHC) strategies and national budgets to make care affordable and accessible.
- Examples of Investment Cases for Sexual Reproductive Maternal Newborn and Child Health (SRMNCAH) include: Small Island Developing States, Lao PDR and Malaysia.
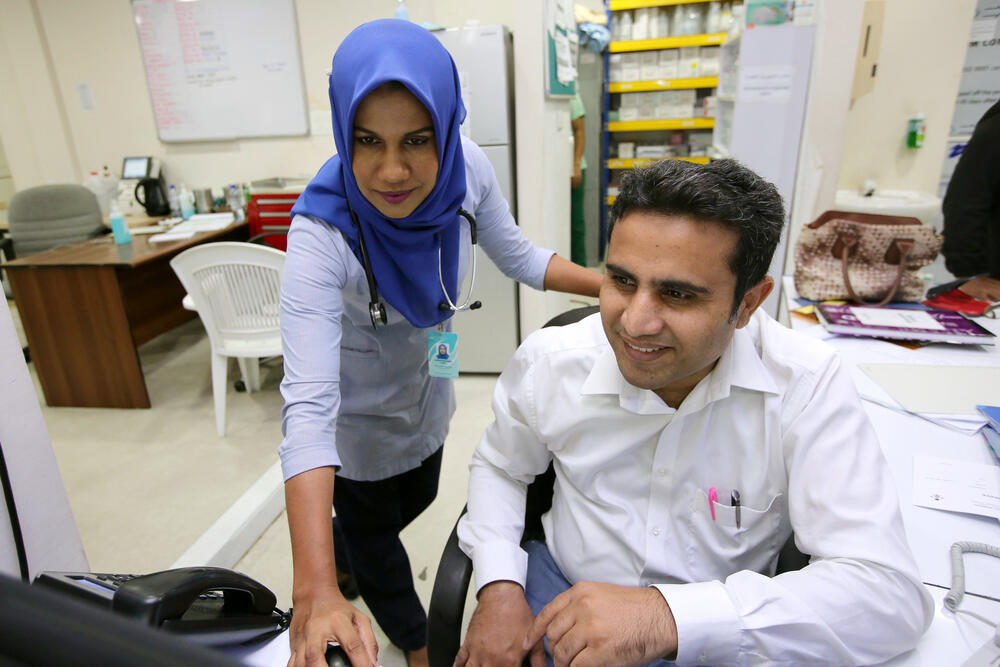
Priority 2: Deliver Quality Health Services

UNFPA helps countries deliver accessible, high-quality integrated maternal health services, and ensure a resilient and well-trained workforce, particularly in fragile and humanitarian settings.
Scaling Up Emergency Obstetric and Newborn Care
UNFPA works to ensure that every mother can reach a facility equipped to provide Emergency Obstetric and Newborn Care (EmONC) within two hours. We use innovative tools like the EmONC Light Assessment Tool (LAT) and GIS-based Travel Time Estimation to find service gaps and strategically place life-saving resources in countries like Indonesia, Cambodia, Lao PDR, Nepal, and Timor-Leste.
Midwifery Capacity Building
In partnership with global experts, we organize specialized EmONC trainings that cover life-saving skills like managing Postpartum Hemorrhage (PPH) and eclampsia in countries of Asia and the Pacific region. Other training provided to midwives and health workers includes: Respectful Maternity Care (RMC), Disability Inclusive Maternal Healthcare, Caring for Pregnant Adolescents, and Perinatal Mental Health.
Building Climate Resilience
Climate change is a growing threat that directly impacts the health of mothers and newborns. UNFPA is undertaking research to understand these effects, including increased mental health issues after natural disasters, and how health centres, staff, and midwives must adapt to deliver essential care.
UNFPA’s practice response, the "Managing Heat Stress in Pregnancy" training package, equips healthcare providers with the skills to treat heat-related illness and advocate for safer, more resilient health facilities.
Tackling Reproductive Morbidities
UNFPA’s work extends beyond immediate childbirth risks to address reproductive morbidities, long-term, debilitating conditions that undermine women’s health, dignity, and quality of life. UNFPA integrates prevention, early detection, and comprehensive treatment into our maternal health services, ensuring women not only survive childbirth but are also empowered to thrive.


Priority 3: Empower Women and Communities

This priority focuses on moving beyond survival to ensuring women thrive, protecting their physical, mental, emotional, and social wellbeing.
Championing Respectful and Rights-Based Care
We believe respectful maternal care is a right for all pregnant women. Addressing the issue of mistreatment is done through numerous channels. We developed and implemented Continuing Professional Development (CPD) courses on Respectful Maternity Care (RMC)/Obstetric Violence to address the mistreatment of women during childbirth. We are also working to incorporate respectful newborn care and bereavement care into training packages.
Addressing GBV and Mental Health
We train midwives to provide first-line psychosocial support for survivors of violence using the LIVES framework (Listen, Inquire, Validate, Enhance safety, Support) and equip them with skills to support women facing loss through our widely-used Perinatal Mental Health course.
Supporting Vulnerable Women
We specifically target marginalized groups with tailored training, including the Caring for Pregnant Adolescents Workshop Toolkit and the Disability Inclusive Maternal Health Care course, emphasizing respectful, inclusive, and equitable care.
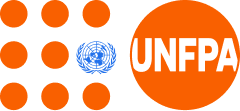
Priority 4: Leverage Data for Impact and Accountability
Reliable data is crucial for planning, measuring progress, informed decision-making, and holding health systems accountable. UNFPA strengthens data quality and use at each level of the health system.
MPDSR and Quality Improvement
We support the establishment and scaling up of Maternal and Perinatal Death Surveillance and Response (MPDSR) systems. MPDSR is the critical mechanism that links every maternal and perinatal death to modifiable factors within the health system, ensuring accountability and driving immediate, life-saving interventions.
Strengthening Data Systems (HMIS)
Our programs focus on enhancing the capacity of health workers and district managers to integrate, analyze, and use key data on SRMNCAH - including from EmONC assessments and MPDSR reviews - within the national Health Management Information Systems (HMIS), promoting evidence-based planning.
Data for Equity
Our aim is to strengthen data capacity to identify vulnerable populations, such as adolescent girls, whose specific needs are often obscured in aggregated national data, reinforcing the mandate to leave no one behind.
Partner with UNFPA: Invest in a Safe Future
Investing in our midwifery-focused models of care is the most cost-effective and essential solution to save and improve the lives and wellbeing of women and newborns. Our strategic approach aligns resources around the global priorities of Commit, Deliver, Empower, and Leverage Data to transform health systems and accelerate progress towards SDG 3.1.
Key institutional partners include the EWENE partnership, WHO and UNICEF, who collaborated with UNFPA and ICM to release the Framework for Action: Strengthening Quality Midwifery Education for Universal Health Coverage (UHC) 2030.
Maternal Health Toolkit and Resources
UNFPA APRO serves as a regional hub for expertise, developing and disseminating technical tools, evidence-based training packages, and policy briefs essential for realizing the Start with Her strategy.
Policy and Guidance Documents
These core documents provide the mandates, strategic frameworks, and technical norms that guide our regional maternal health priorities:
- The Campaign to End Fistula: 10 years On
- ICM Essential Competencies for Midwifery Practice (ICM)
- ICM Global Standards for Midwifery Education (ICM)
- International Definition and Scope of Practice of the Midwife (ICM, 2023)
- Philosophy and Model of Midwifery Care (ICM)
- Implementation Manual for Developing a National Network of Maternity Units
- Implementation Manual for Developing a National Network of Maternity Units: Improving Emergency Obstetric and Newborn Care (EmONC)
- Maternal and Perinatal Death and Surveillance and Response: Materials to Support MPDSR Implementation
- Policy Brief: Quality Midwifery Education
- Strategies toward ending preventable maternal mortality (EPMM)
- Strengthening quality midwifery education for Universal Health Coverage 2030: Framework for action
- Taking Stock: Sexual and Reproductive Health and Rights in Climate Commitments
- The Global Midwifery Accelerator (2025)
- Transitioning to midwifery models of care: global position paper (WHO, 2024)
UNFPA Key Publications and Reports
These publications provide the essential data and evidence base for our advocacy, program design, and monitoring efforts:
- 2024 Orange Book of Results (Key Results Achieved at the Country Level)
- Cervical Cancer Policy Briefs
- Maternal and Newborn Health Fund Annual Impact Report 2024
- Maternal mortality levels and trends (WHO)
- Social Determinants of Maternal Death and Disability
- State of Asia’s Midwifery 2024 Report and Infographic
- State of the World’s Midwifery 2021
- State of World Population Report 2024 (Interwoven Lives, Threads of Hope)
- Taking Stock: SRHR in Climate Commitments
- Technical brief and action plan on adolescent pregnancy in South Asia
- The Real Fertility Crisis: The pursuit of reproductive agency in a changing world
- Trends in maternal mortality estimates 2000 to 2023
- UNFPA Asia and The Pacific: Brief about our work
- UNFPA Asia and the Pacific Annual Report 2024
- UNFPA Counting What Matters 2022
- UNFPA Strategy for Reproductive, Maternal and Newborn Health and Well-Being 2025–2030 (Start with Her)